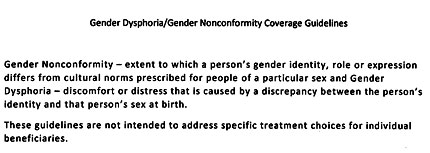
This week, Rhode Island’s Department of Health and Human Services announced that the state’s Medicaid program has removed arbitrary and outdated coverage exclusions for transgender Rhode Islanders. The new guidance can be read here.
All major national medical and mental health experts, including the American Medical Association, the American Psychological Association, and the National Association of Social Workers, have affirmed the medical necessity of providing transition-related treatment for transgender people. Rhode Island is the 10th jurisdiction to update its Medicaid policy to include medically necessary treatments for its transgender policyholders, joining California, Maryland, Massachusetts, Oregon, Vermont, Connecticut, Washington, New York, and Washington D.C. [pullquote]Rhode Island is the 10th jurisdiction to update its Medicaid policy to include medically necessary treatments for its transgender policyholders, joining California, Maryland, Massachusetts, Oregon, Vermont, Connecticut, Washington, New York, and Washington D.C. [/pullquote]
“This change will allow many people to get the care they need. It’s an important step towards addressing the healthcare disparities that impact trans* Rhode Islanders,” said Ethan Huckel of TGI Network. “We applaud HHS Secretary Elizabeth Roberts and Governor Gina Raimondo for their leadership in bringing our Medicaid policy up to date and ensuring that every Rhode Islander has the potential to live a happy, healthy, and productive life.”
“The guidance will be life-saving for transgender Rhode Islanders on Medicaid,” said Jennifer Levi, director of the Transgender Rights Project for Gay & Lesbian Advocates & Defenders (GLAD). “Unfortunately, all too often transgender people cannot get insurance programs to cover essential medical services. This guidance should change that.”
While the policy has expanded coverage, it does not address the surgical needs of transgender people under the age of 18; electrolysis, which is often a pre-surgical requirement, or Facial Feminization Surgery (FFS) which is needed for true parity between services offered for trans men and those offered for trans women.
Additionally, private health insurance companies in Rhode Island, regulated by the Office of the Health Insurance Commissioner, are not under the same purview as Medicaid and most plans still include discriminatory outdated coverage exclusions for transgender policyholders.
“Since Rhode Island’s nondiscrimination law was updated in 2001 to ban discrimination on the basis of gender identity and expression, we are hopeful that the Office of the Health Insurance Commissioner will soon follow suit and issue a public bulletin barring gender identity-based discrimination in private insurance plans,” said Huckel.
TGI Network of Rhode Island is the only all-volunteer, statewide organization dedicated to providing support and advocacy for the transgender, gender-variant, and intersex (TGI) community in Rhode Island and surrounding areas. Our mission is to serve the needs of the TGI communities in Rhode Island and surrounding areas through support, advocacy, and education.
Through strategic litigation, public policy advocacy and education, Gay & Lesbian Advocates & Defenders works in New England and nationally to create a just society free of discrimination based on gender identity and expression, HIV status and sexual orientation.
[From a News Release]